What are inhibitors?
One complication that can happen to some people with hemophilia is developing “inhibitors.” Inhibitors are antibodies that are produced by the body’s own immune system.
Normally, your immune system helps protect your body against disease and infection by producing antibodies. Antibodies recognize and destroy any “foreign” substance that doesn’t belong there, such as viruses or bacteria.
In the case of hemophilia, the “foreign” agent being destroyed is factor VIII or IX, in hemophilia A and B respectively. Inhibitors against factor VIII typically develop during the first 50 treatments of factor replacement therapy in people with severe hemophilia A.
How do inhibitors work?

When the blood product is injected into the body, these inhibitors attack the factor proteins and destroy them, rendering them ineffective. Without these proteins, the “clotting cascade” isn’t able to produce a clot. This means that patients with inhibitors have little to no protection against bleeds and will need alternative treatment in the event of an active bleed.
Select an option to see how the clotting cascade is affected.
12
11
9
8
10


12
11
9
10
12
11
9
8
10


12
11
9
8
10

Adapted from AboutKidsHealth.ca
How common are inhibitors?

Hemophilia A and factor VIII inhibitors
Inhibitor development is more common in hemophilia A, occurring in up to 30% of people with a severe form of the disease. Most people develop inhibitors when they are young children in the days and weeks following their first factor VIII infusions.

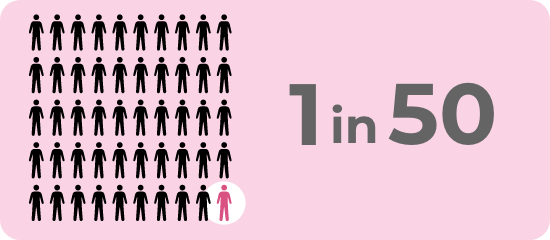
Inhibitors can also affect people with mild and moderate hemophilia A. About 1 in 50 people will develop this complication, typically during adulthood.
Hemophilia B and factor IX inhibitors
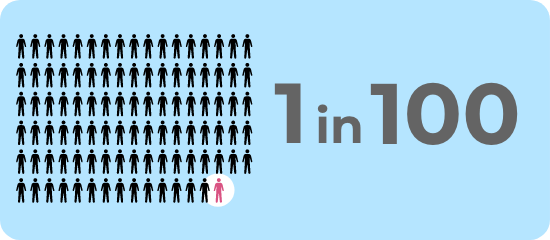
Inhibitors are much less common in hemophilia B, only affecting about 1 in 100 people. Similar to hemophilia A, most inhibitors typically occur before the first 20 exposures. Inhibitors to factor IX are associated with a risk of severe, anaphylactic reactions following administration.
Are there risk factors associated with developing FVIII inhibitors?

Some contributing factors to inhibitor development include:
- Certain genetic mutations
- Family history of inhibitors
- Ethnicity – black African or Hispanic ancestry
- High-intensity factor exposure (e.g., surgery or trauma requiring high dose factor replacement)
When should inhibitor screening occur?

Likelihood of Developing an Inhibitor
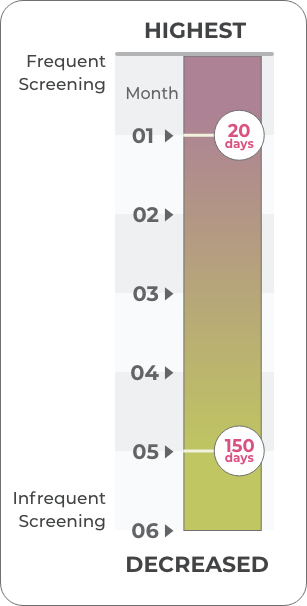
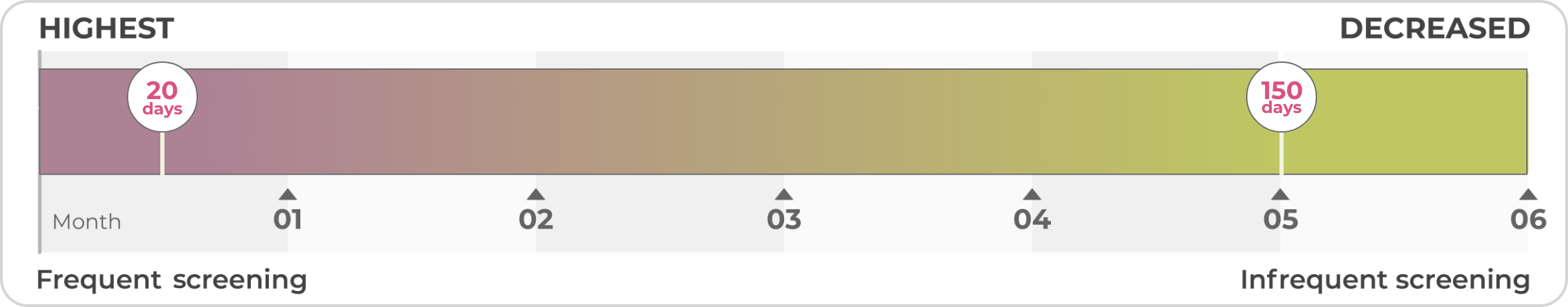
The highest incidence of inhibitor development occurs during the first 20 exposure days to factor.
- This can occur when children are receiving treatments on demand, or may occur after they have started a prophylaxis regime.
- These children should be monitored frequently for inhibitor development.
Adults with more than 150 treatment exposure days need less frequent screening.
Other situations in which inhibitor screening should be considered include:
- After initial factor exposure
- After intensive factor exposure, e.g., daily exposure for more than 5 days
- Poor or no response to adequate factor replacement therapy
- Before surgery
- For suboptimal post-operative response to factor replacement therapy
Many hemophilia treatment centres do inhibitor screening on an annual basis.
When inhibitors are initially detected, a management plan needs to be put into place quickly for optimal care and prevention of serious or fatal bleeds. Your hemophilia treatment team is experienced in dealing with inhibitors and will create a plan of care tailored to you.
Are there different types of inhibitors?

Inhibitors come in different degrees of severity. They are measured in what is called Bethesda Units (BU). The greater the number of BU, the more inhibitors are present in the body.
Low-titre inhibitors (LTI)
- Inhibitors are present at less than 5 BU
- Transient
- May resolve spontaneously without treatment, require frequent monitoring
- Can progress to a high-titre inhibitor
High-titre inhibitors (HTI)
- Inhibitors are present at levels greater than 5 BU
- Persistent
- Bleeds do not respond to infused factor concentrates
- Factor is destroyed, rendered ineffective
Are there treatments for inhibitors?

If an inhibitor is detected, your treatment team will classify it as an LTI or an HTI. Keep in mind that titre levels can fluctuate and be more active at certain times than others. Treatment options differ depending on how the inhibitor is classified.
LTIs don’t always require treatment.
Immune Tolerance Induction (ITI) Therapy
Goal: eradicate inhibitors
- Large amounts of factor concentrate are given daily or several times per week
- Ideally, this high exposure will help your immune system accept that factor is not harmful to the body and will stop the immune system from producing antibodies that destroy it
- Treatment typically lasts months to years
- Not as effective in hemophilia B
Bypassing Agents
Goal: prevent and treat bleeds
- Recommended for people with HTI
- Instead of replacing the missing factor, bypassing agents go around (or bypass) the factors that are blocked by the inhibitor to help the body form a normal clot
- Dosing frequency varies, depending on the different types of hemorrhages and/or if it is being used routinely to prevent bleeding episodes
- Close monitoring of people taking bypassing agents is important
Non-factor Therapies
Goal: prevent bleeds despite active inhibitors
- Agents that mimic the function of factor VIII but aren’t affected by inhibitors in hemophilia A
- Other non-factor therapies are also in various stages of development. These molecules are designed to substitute for FVIII in the clotting cascade, but are completely different to FVIII
Clotting Factor Concentrate
- Unlike for people with HTIs, factor replacement, albeit at much higher doses (typically 3-fold higher) may still be used to treat bleeds in people with LTIs.
Talk to your healthcare team if have any questions about screening and managing inhibitors.

