Head injuries are a serious concern in patients with hemophilia or other bleeding disorders. A head injury can affect anywhere from the outermost layer of the head, the scalp, all the way down into the brain tissue, and can occur at any age. Head injuries can range in severity from superficial bumps and bruises to bleeding within the brain and its protective layers.
Head Bumps
Bumps to the head often result in a “goose egg” , which is a swelling of the scalp caused by trauma to the skin and broken blood vessels. Goose eggs may take a bit of time to go away, but they aren’t serious.
Toddlers heads tend to be large in proportion to the rest of their body. As they become preschoolers, they’ll be active and develop new motor skills. This may lead to falls and bumps as they practice these skills.
Children with a bleeding disorder who experience any type of bump to the head should be immediately assessed in the ER. Even if the injury looks to be superficial, the only way of determining the extent of the injury is to have it assessed by a medical team.
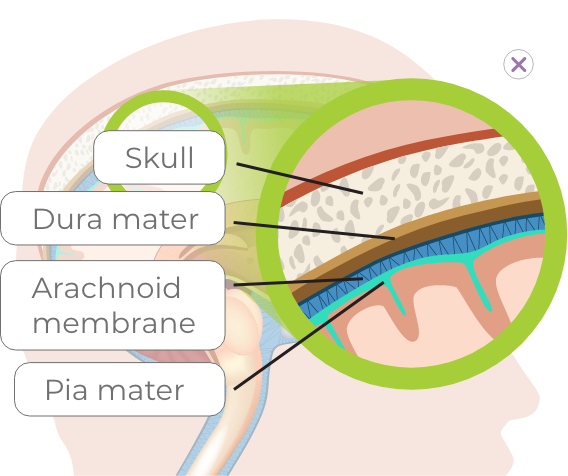
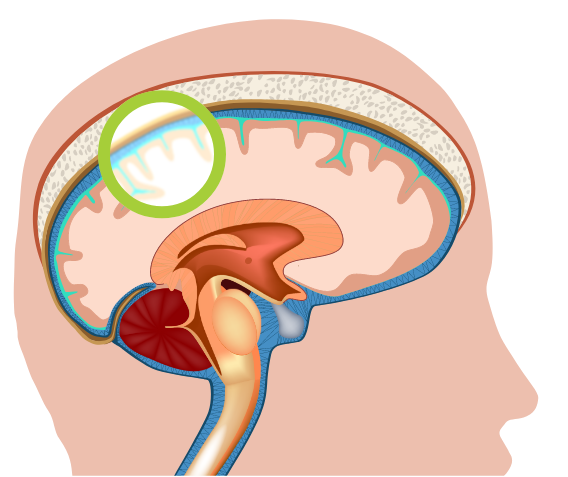
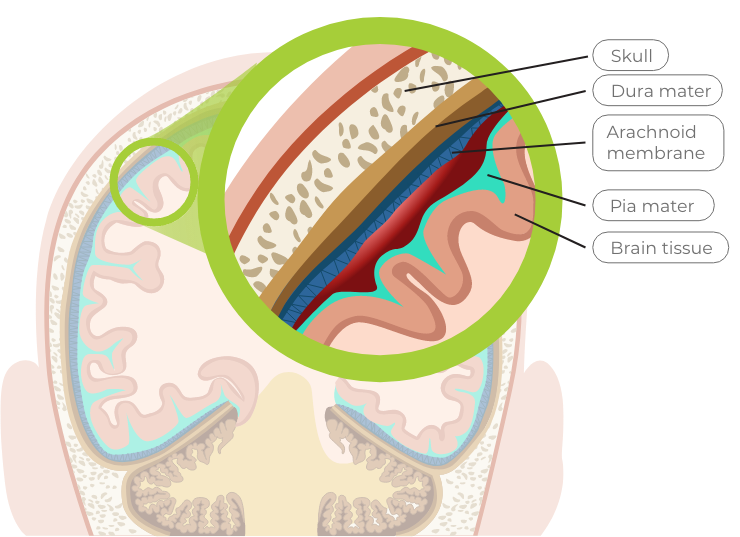
Anatomy of the protective layers of the brain
The brain is protected by the outermost layer of tissue which is the scalp, followed by the bony skull. The brain is suspended in cerebrospinal fluid (CSF). There are 3 protective layers called the meninges that cushion the brain and CSF within the skull. The three layers of the meninges are the dura mater, arachnoid membrane, and pia mater. Their role is to cover and protect the brain.
Click on the diagram to see more detail.
Types of Brain Bleeds
Brain bleeds have a number of causes, including head trauma resulting from a fall or a heavy blow to the head.
There are 2 main types of bleeds that can occur within the skull. These are known as intracranial hemorrhage and they are classified as follows:
- Bleeding that occurs inside the brain tissue (intracerebral or intraventricular hemorrhage), or
- Anywhere between the three protective layers (meninges) – dura mater, arachnoid membrane, or pia mater

Uninjured brain
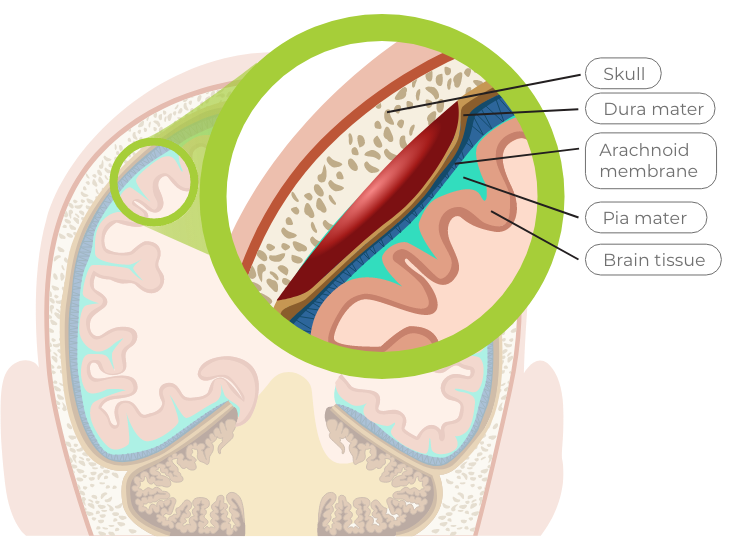
Dura mater
the tough outer layer
A bleed that occurs between the skull bone and the dura mater is called an epidural bleed
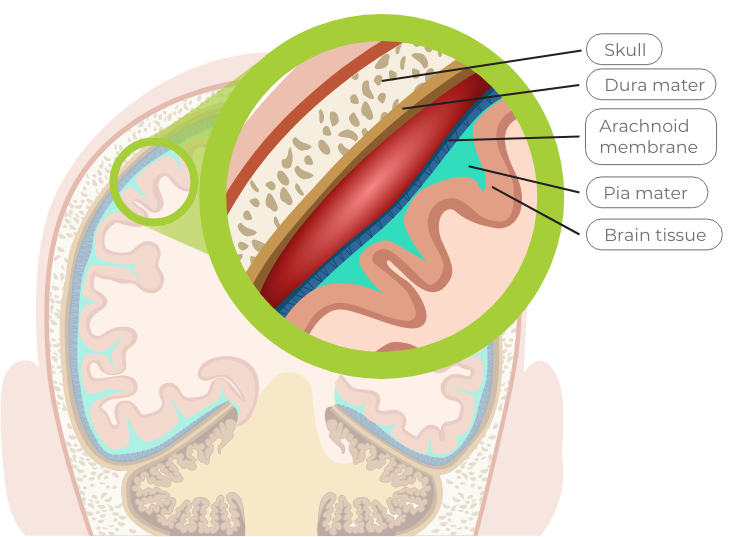
Arachnoid membrane
the middle web-like structure filled with fluid that cushions the brain
A bleed that occurs between the dura mater and the arachnoid membrane is called a subdural bleed
Pia mater
the delicate inner layer
A bleed that occurs between the arachnoid membrane and the pia mater is called a subarachnoid bleed
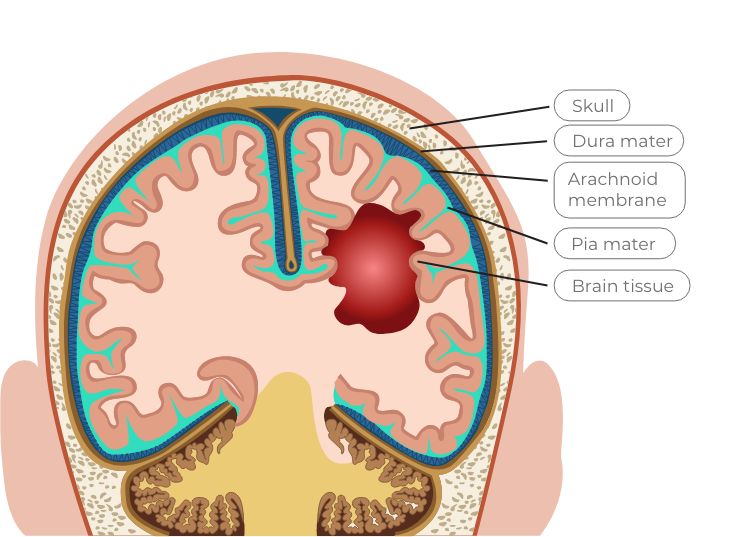
Intracerebral hemorrhage
This bleeding occurs in the lobes, pons, and cerebellum of the brain (bleeding anywhere within the brain tissue itself, including the brainstem)
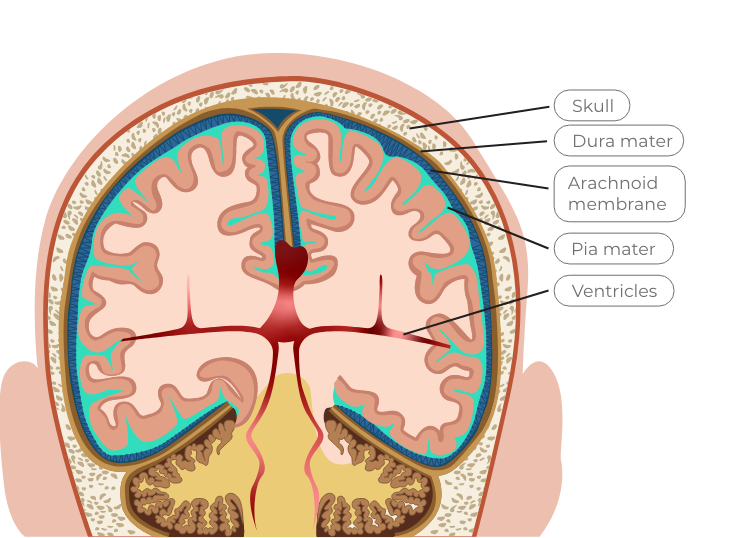
Intraventricular hemorrhage
This bleeding occurs in the brain’s ventricles, which are specific areas of the brain (cavities) where cerebrospinal fluid is produced
Diagnosis
Brain bleeds are diagnosed based on an evaluation of physical symptoms and a number of different tests, including imaging tests such as computed tomography (CT) scan, magnetic resonance imaging (MRI), or magnetic resonance angiogram (MRA). There may not be any obvious signs of a head injury until hours or even days after the injury. Therefore, it is very important that children are monitored for symptoms for up to 2 weeks following the injury.
Monitoring
Signs and symptoms to monitor for include:
- Headache that worsens and isn’t responsive to acetaminophen
- Repeated vomiting
- Seizures
- Loss of consciousness
- Double or blurry vision
- Light sensitivity
- Stiffness of the neck or complaints of pain with neck movement
- Changes in normal behaviour/personality
- Increased sleepiness, difficult to wake from sleep, sluggish
- Dizziness and poor balance
- Lack of coordination, clumsiness
- Sudden weakness
- Slurred speech
- Confusion
If your child experiences a bump to the head and is experiencing any of the above symptoms, they will require immediate medical attention.
Treatment
Any type of bleeding inside the skull or brain is a medical emergency. All head injuries with or without swelling should be treated promptly. The healthcare team will determine the most appropriate treatment.
Steps to Prevent Head Injuries at Different Stages
While many head injuries are preventable, there are risks associated with different age groups and stages of development. Keep in mind that injuries of any type can occur at any age.
Infants and toddlers


While infants and toddlers begin to grow and explore, there are many opportunities for head injuries, such as:
- Rolling off change tables
- Falling down stairs
- Bumping head on cupboards, coffee tables
- Falls from learning to stand and walk
Here are some tips to limit the chances of head injuries in infants and toddlers:
- Install baby gates at the top and bottom of stairs
- Put protective corners on tables
- Carpet hard floors
- Limit tripping hazards, such as throw rugs and toys
- Consider a soft-shelled helmet for toddlers learning to walk (if bleeding disorder is severe)
- Never leave infants unattended, keep a hand on them at all times while on a change table
- Properly fitted car seats
School-age children


Physical activity is so important for school-age children, as it help with their fitness, as well as their social and emotional development. Yet, increased physical activity comes with increased risk, such as:
- Falls while learning to skate, ride bikes, ski
- Injury from winter sliding activities (tobogganing, skating, skiing, snowboarding), slips on ice
- Sport-related head injury
- Falls from playground equipment, trampolines
Some tips to help prevent injuries in this age group include:
- Keep walkways and driveways free of ice
- Wear non-slip footwear (both summer and winter)
- Wear a helmet (tobogganing, downhill skiing, bicycling)
- Children with bleeding disorders should wear a medical alert bracelet
- Avoid trampolines (both indoor and outdoor)
- Receive proper instruction (i.e., take a lesson) if learning a new sport
Teens and young adults


As children grow into teenagers and young adults, their risks for head injuries change. While they are just as likely to slip and fall, they often engage in higher risk activities and typically aren’t monitored as closely by their parents. They often have more confidence in activities they’re doing and take more risks than younger children.
- Motor vehicle accidents
- Highly competitive/riskier sports
- More time spent away from parents
In addition to tips already listed:
- Ensure they have a good understanding of their bleeding disorder and can explain it in the event a parent isn’t present
- Have them carry a Factor First card in their wallet
- Encourage them to stay within their physical limits