People with hemophilia are at risk of developing bleeds into their muscles and joints, even without significant injury to the site.
Repeated bleeds into the same muscles and joints can cause permanent damage over time, therefore, it is important to learn how to identify and treat them early on.
Joint bleed, also called hemarthrosis
A joint is where two or more bones meet and allows for movement. The bones are lined with a thin barrier, called a synovial membrane, that acts to protect and cushion the joints they surround.
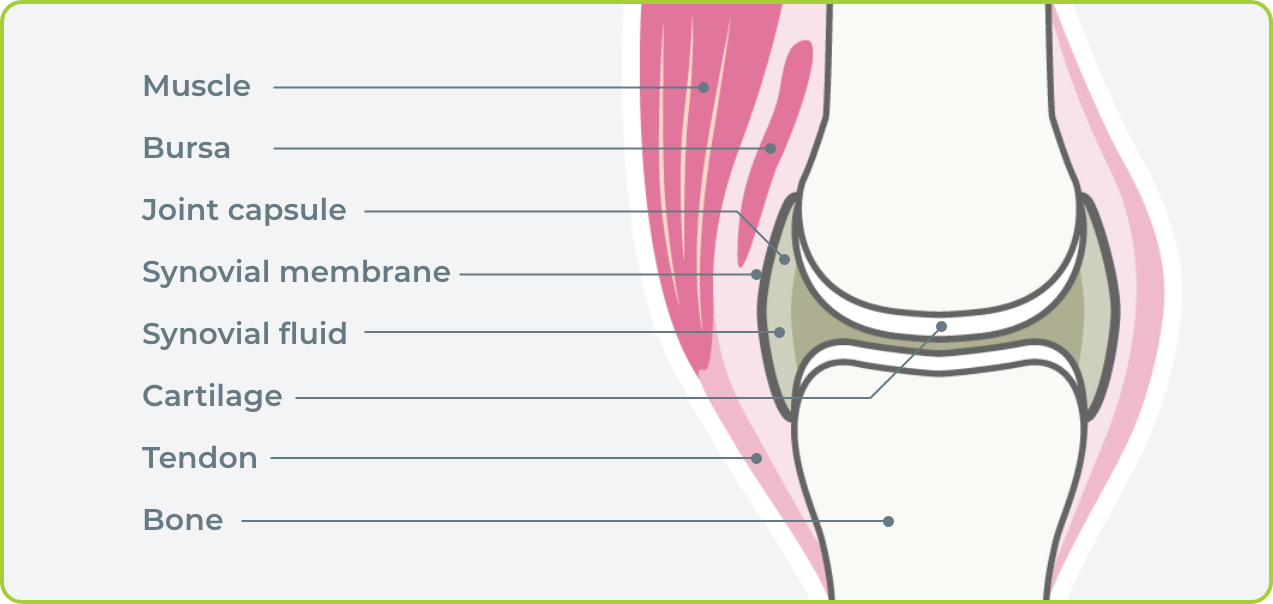
Hemarthrosis happens when a joint bleed occurs and blood seeps into the synovial membrane. Pressure builds within the joint space, causing pain, swelling, and an inability to move the joint properly.
Joint bleeds can occur in any joint in the body, however the knees, elbows, and ankles are the most affected joints.
Joint bleeds often occur in people with hemophilia after trauma to the area. Unfortunately, people with severe hemophilia can experience joint bleeds from little to no trauma at all. These are called spontaneous joint bleeds.
Repeated bleeds to the same joint cause permanent damage over time. If joint bleeds are not treated, they could lead to one or more of the following:
- loss of movement
- joint arthritis
- arthropathy (meaning “degeneration of a joint” – the joint surfaces become worn, and the joint can be stiff and painful)
- chronic pain
- trouble with daily activities and mobility
- muscle weakness
Signs and symptoms of a joint bleed
Symptoms of a joint bleed aren’t always apparent right away.
In children, parents may recognize some early signs of joint bleeds. For example, a parent may notice that the child is limping, or having difficulty moving a limb.

The person with the bleeding disorder will notice:
- stiffness or a "tingling" sensation
- discomfort at rest and with movement
Swelling may not be obvious immediately, so it is important to look for:
- warmth over the joint
- the joint feels warmer compared to surrounding tissues
- loss of motion compared to the opposite arm or leg OR the usual amount of motion
- tenderness to touch
Swelling, pain, and possible redness may occur if the bleeding continues.
It is very important to identify early to prevent the extent of damage and symptoms. Repeated bleeds into the same joint can lead to target joints. These joints become permanently damaged and tend to re-bleed with minimal trauma.

Muscle bleed
Bleeding into muscle is a type of bleed called a soft tissue bleed. Muscle bleeds are less common than joint bleeds. Muscle bleeds can be more serious than joint bleeds because of their complications.
Bleeds can occur in any muscle in the body, and commonly result from slips, falls, collisions with another person or hard object, repeated motions over and over, lifting or moving something that is too heavy.
A muscle bleed occurs when muscle fibers are torn. Outside swelling is not always initially obvious in some large muscles because the blood is not contained to a single area and can seep slowly through different layers of the muscle.
Deeper muscles are wrapped in a tissue called fascia, forming compartments. Bleeding into these deep muscles quickly fills the compartments and can cause pressure on the nerves and blood vessels in the compartments, leading to muscle damage.
Signs and symptoms of a muscle bleed
Similar to a joint bleed, a parent may notice that the child is limping or having difficulty moving their limb.
Early symptoms of a muscle bleed may include:
- discomfort and feeling of stiffness or tingling
- pain if the muscle is stretched
- pain if the muscle is contracted (made to work)
Swelling may not be immediately apparent, so look for warmth and tenderness.
Later symptoms of a muscle bleed may include:
- pain even when the muscle is resting
- firm, tender swelling in the muscle
- pins and needles, tingling or numbness
- when bleeding puts pressure on a nerve, your leg or arm may "go to sleep"
- the skin over the muscle changes color or becomes blue
- the veins in your arms or legs look bigger than usual
Contact your healthcare team if any of these later signs are present.
TREATING A JOINT OR MUSCLE BLEED
If you suspect a joint or muscle bleed, inform your hemophilia treatment centre. A member of your healthcare team will provide specific guidance on how to manage the bleed.
When a joint or muscle bleed has occurred, follow these recommended first aid principles.
Rest
Do not use the joint or muscle while it is painful or swollen. Use crutches or a wheelchair when there is a joint or muscle bleed in the leg. Use a sling to rest arm bleeds.
Ice
Ice may help to decrease pain. Use an ice pack, gel pack or crushed ice.
For small joints, leave the ice on for 5-10 minutes.
For larger joints or large muscle bleeds, up to 20 minutes may be needed. Reapply the ice every two hours for the first two to three days, or until the pain has decreased.
Do not use ice if it is making the pain worse.
Immobilization
If the joint is very swollen or if movement is lost, a splint or half cast may be used to protect the joint.
If there is a lot of pain and loss of motion, a splint or half cast may be used to allow the muscle to relax.
Compression
Compression limits the amount of bleeding.
A tensor bandage or an elastic sleeve will support the joint and help to control the swelling, however, compression may not be tolerated if the joint is very tender.
A tensor bandage or compression with padding may be used to compress the muscle and help to control the swelling.
Circulation must be watched carefully; if there is any numbness or tingling, or if the pain is increasing, remove the compression immediately and notify your healthcare team.
Elevation
Keeping the injured part six inches above the level of the heart will decrease the pressure on the damaged blood vessels and help slow the swelling. Elevate the area often for the next 2 to 3 days while resting or follow recommendations from your medical provider.
In general, work with your healthcare team and physiotherapist trained in Hemophilia care to rehabilitate the joint or muscle. The treatment plan that your healthcare team recommends should be continued until the joint or muscle is healed completely and its strength restored. Contact your healthcare team and physiotherapist for recommendations before you go back to regular activities, including sports or work.

